Thyroid Eye Disease Treatment, London
The Ezra Clinic is a global leader in oculoplastic surgery dedicated to improving lives through innovative Thyroid Eye Disease (TED) care. Our clinic thrives on a holistic, team-based approach, integrating the expertise of renowned surgeons, immunologists, radiologists, and endocrinologists.
We specialise in the latest biological treatments for active TED and offer comprehensive surgical rehabilitation featuring blepharoplasty, orbital decompression, and advanced skin treatments. At Ezra, every patient's experience is filled with cutting-edge solutions and genuinely compassionate care, aiming to achieve the best possible outcomes and enhance the quality of life.
This lady presented with severe thyroid eye disease. She demonstrates typical changes including lid retraction, bulging eyes and eyelid bags. She was treated initially with an orbital decompression to restore the position of the eyes.
This was followed by upper and lower lid blepharoplasty with midface lift to restore the cheek volume and smooth interface with the eyelid. The results were transformational as seen in the before and after eyelid treatment pictures, with a very positive impact on the patient’s quality of life.

What is Thyroid Eye Disease?
Thyroid Eye Disease (TED) is an autoimmune inflammatory condition of the eye socket. TED is also commonly known as Graves’ Orbitopathy (GO), and it affects the muscles and fatty tissue behind the eyes, causing them to become swollen, red and inflamed. This eye disease can affect patients in many ways as it often makes the eyes feel gritty and swollen, but in more severe cases, it can affect the vision and cause facial disfigurement. Fortunately, there are effective medical and surgical treatments for the different stages and types of TED.

An example of the mixed changed associated with thyroid eye disease. This patient has left upper lid retraction, fullness of the eyelids and disordered eye movements leading to double vision.

One of the most debilitating symptoms of Thyroid Eye Disease is double vision. This occurs because some of the muscles that move the eye became scarred and fixed, meaning that the eyes can point in different directions. This patient is attempting to look upwards, but the scarred muscles on the left eye prevent movement.

This patient shows quite typical features of TED. The eyes are proposes (bulging forward due to expansion of the fat behind the eye.) There is also marked upper eyelid retraction keeping the upper eyelid in a very high position. This combination of features contribute to an ‘angry’ look which TED patients often complain of.
Another example of typical TED symptoms, including bulging eyes due to fat expansion behind the eye and significant upper eyelid retraction, resulting in an 'angry' appearance frequently reported by TED patients.

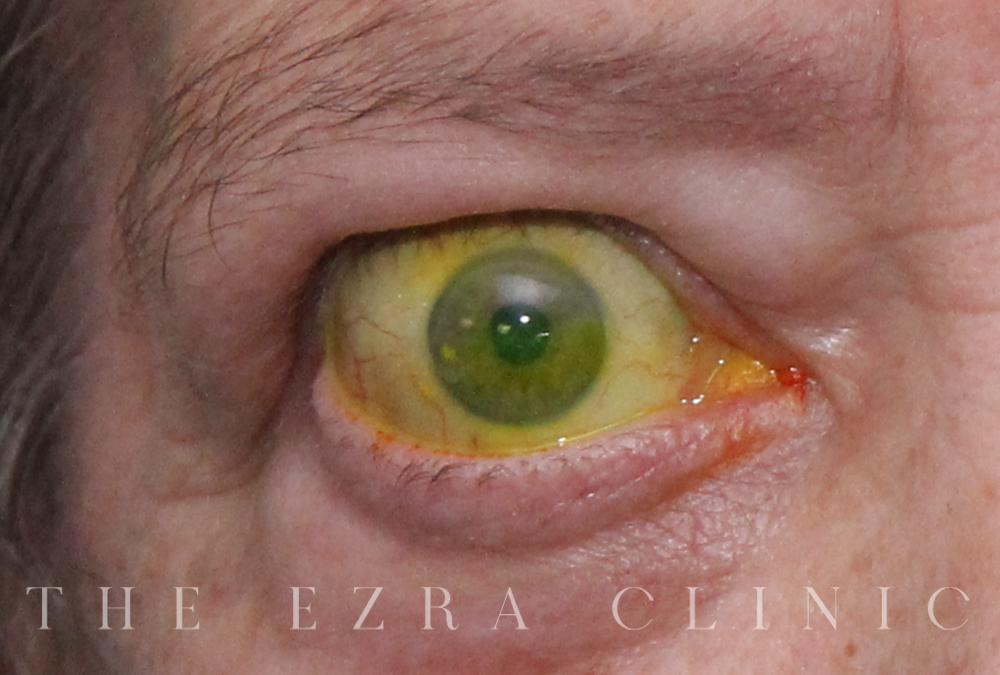
This image is of a patient with highly active thyroid eye disease. The typical features of proptosis (bulging eyes), fullness of the eyelids and redness are all visible here. This patient was managed with medication only and made an excellent recovery

Causes of Thyroid Eye Disease
Thyroid eye disease is commonly caused by hyperthyroidism associated with Graves' disease, though it can occur in other contexts. It is not shared and has an incidence of around 19 per 10,000.
TED may affect any age group and most frequently occurs in the working-age population, specifically women. It may also affect patients during pregnancy.
THYROID EYE DISEASE SYMPTOMS
In the earlier stages It is frequently misdiagnosed as other conditions, such as allergic eye disease, hay fever or dry eye.
Therefore, it commonly requires specialist expertise to give an accurate diagnosis. However, symptoms of thyroid eye disease depend on the severity of the condition.
One of the most debilitating symptoms of Thyroid Eye Disease is double vision. This occurs because some of the muscles that move the eye become scarred and fixed, meaning that the eyes can point in different directions.
Common milder symptoms:
- Ocular irritation
- Swelling around the eyes
Severe symptoms:
- A feeling of eye grittiness
- Swelling in upper eyelids
- Eye bags
- Redness of eyelids
- Sensitivity to light
- Blurred or double vision
- Dry or watery eyes
- Bulging eyes (giving a 'staring' look)
- Pain and discomfort
- Finding it hard to move the eyes
- Sight loss
Most severe symptoms:
- Threatens vision
- Blindness due to compression of the optic nerve behind the eye
- An inability to close the eyes, leading to corneal exposure
How is TED diagnosed?
People with thyroid problems, particularly those with overactive thyroid function, should be mindful of the increased possibility of developing the disease. A GP should explain the symptoms to look out for. However, TED can occur after or before a thyroid problem is detected, which is why many people are misdiagnosed and only go on to develop mild thyroid eye disease symptoms. Your GP should refer you to a specialist ophthalmologist (eye doctor) who may work with an endocrinologist (hormone specialist) to help manage the condition and live a happier life.
The ophthalmologist can diagnose thyroid eye disease by conducting a comprehensive eye examination, arranging specialised blood tests and requesting orbit scans, such as a CT or MRI if necessary.
Thyroid eye disease can be complicated and affect people differently. Many factors require detailed consideration, including:
- Thyroid hormone control
- An accurate ophthalmic assessment
- A review of orbital imaging
- The delivery and management of medication and immunosuppression in some patients
- The selection of patients for surgery before surgical therapy
At The Ezra Clinic, we offer a dedicated multidisciplinary service where specialists from different areas come together to discuss and review your situation to deliver the best possible care. We meet regularly to review your results, scans and photos to plan ongoing solutions as part of a multidisciplinary team. This unique team-based approach ensures that you are in the best possible hands and have the best possible treatment.

Stages of thyroid eye disease
There are two phases to Thyroid Eye Disease: the active phase and the inactive phase.
Early active phase
The early active phase means the disease is progressing actively. It is characterised by inflammation, often lasting six months to two years.
It is essential to restore lubrication during the active phase as the eye's surface dries out since the eyelids are tight and cannot blink properly. The inflammation may also cause the tear glands to produce fewer tears. Many patients say that they feel a burning sensation around the eyes, or even a dull ache that can be worse when moving the eyes.
Treatment for early active phase
Some tips to help alleviate Thyroid Eye Disease symptoms include:
- Using liquid teardrops (or artificial tears) offer significant relief
- Wearing wrap-around sunglasses if your eyes are sensitive to light, wind, or other irritants
- Avoiding extreme temperature
At the Ezra Clinic, we offer a wide range of treatments for the Active Phase according to each individual case, such as steroids.
Inactive or chronic phase
The inactive phase is when TED has "burnt out". Unfortunately, patients may have to be content with changes that occur in their appearance as these may be mild or, in some cases, may result in significant disfigurement and double vision.
Treatment for inactive phase
The objective is to reverse the changes that may have occurred. This is a common surgical procedure that may need a variety of therapies, such as orbital decompression, eyelid lowering, blepharoplasty, or a combination of all the above.
Orbital decompression surgery
Orbital decompression helps treating patients with proptosis (bulging eyes) due to thyroid eye disease (TED). This is where the muscles and/or other tissue connected to the eye gets too big for the holes in the skull where they sit. It is designed to remove bone and/or fat, the amount of proptosis from behind the eye that can cause problems such as vision loss. Orbital decompression surgery increases the space for these muscles and/or tissue, which helps reduce the proptosis\'s effect.
TYPES OF ORBITAL DECOMPRESSION SURGERY
Lateral wall decompression
A 10 to 5 mm long incision is made in the ‘laughter line’ of the outer eyelids, and a section of bone behind the outer wall of the eye socket is removed. The skin is closed with a few stitches, which are removed after two weeks.
Medial (inner) wall decompression
A small incision is made behind the inner corner of the eyelids to remove the inner wall of the eye socket and the sinuses. The incision leaves no visible external scar. Alternatively, the medial wall can be removed through the nose (endonasal medial wall decompression).
Orbital floor
A portion of the floor of the eye socket beneath the eyeball can be removed via a lateral wall approach or a medial wall approach, as the nerve to the cheek runs through the bone of the floor. The surgery can sometimes affect it, accounting for the numbness that often follows, but it typically improves with time.
Balanced two-and-a-half wall decompression (lateral and medial walls)
It combines the medial and lateral wall decompression and some of the orbital floor as above.
Fat decompression
Since thyroid eye disease is often associated with increased orbital fat during surgery, fat may be removed through one of the bony openings to further decompress the orbit.

This patient has isolated left upper lid retraction as a result of the TED. After medical treatment, the residual retraction was treated with an eyelid lowering procedure, performed through the inside of the eyelid, meaning that there were. No scars of the skin. The surgery is minor and performed as a daycare. The after surgery images demonstrate a significant improvement in the symmetry and an alleviation of the dry eye was also experienced.
Potential risks and complications
Orbital decompression is a major surgery and should only be considered after consulting with one of our specialists.
Some of the risks include:
- Infection and bleeding are rare complications
- A fine line scar is hidden within the ‘laughter lines’ of the outer corner of the eyelids
- Swelling of the upper and lower eyelids that settles over a few months
- A ‘wobble’ of the vision on eating (‘masticatory oscillopsia’) occurs in about 40% of patients but quickly settles in nearly all patients • New onset (beginning of) double vision is rare with a lateral wall decompression.
- Blindness but it is extremely rare
Remember that the benefits of surgery generally outweigh the risks. One of our surgeons will discuss this with you in more detail before you undergo surgery.
Preparation for the surgery
To be prepared and recover smoothly, we advise not to take aspirin, aspirin-type medications, or anti-inflammatory medicines for three weeks before surgery.
Patients on other blood-thinning medications should be stopped according to local anti-coagulation protocols before surgery, as your GP or cardiologist advises. We will provide further advice at your consultation.
In addition, the surgery is usually performed under a general anaesthetic so the patient will not feel pain.
After surgery care
Following your surgery, eye pads are placed over the operated eye(s) and gently removed the next day before leaving the hospital. In addition, taking mild pain relief medication is recommended for some discomfort after the surgery.
Other recommendations include:
- Sleeping on an extra pillow at night to help reduce swelling and bruising that should settle within a few weeks of surgery
- Taking at least two weeks off work
- Avoid nose-blowing, flying, and scuba-diving for at least three weeks.
- Avoid driving if you experience new or worsening double vision.
If you have medial wall decompression; drainage of the air sinuses around the eye may be temporarily affected. Rarely, however, sinus symptoms can continue following your surgery, and this may need medical or surgical treatment.