BASAL CELL CARCINOMA (BCC) OF THE EYELID
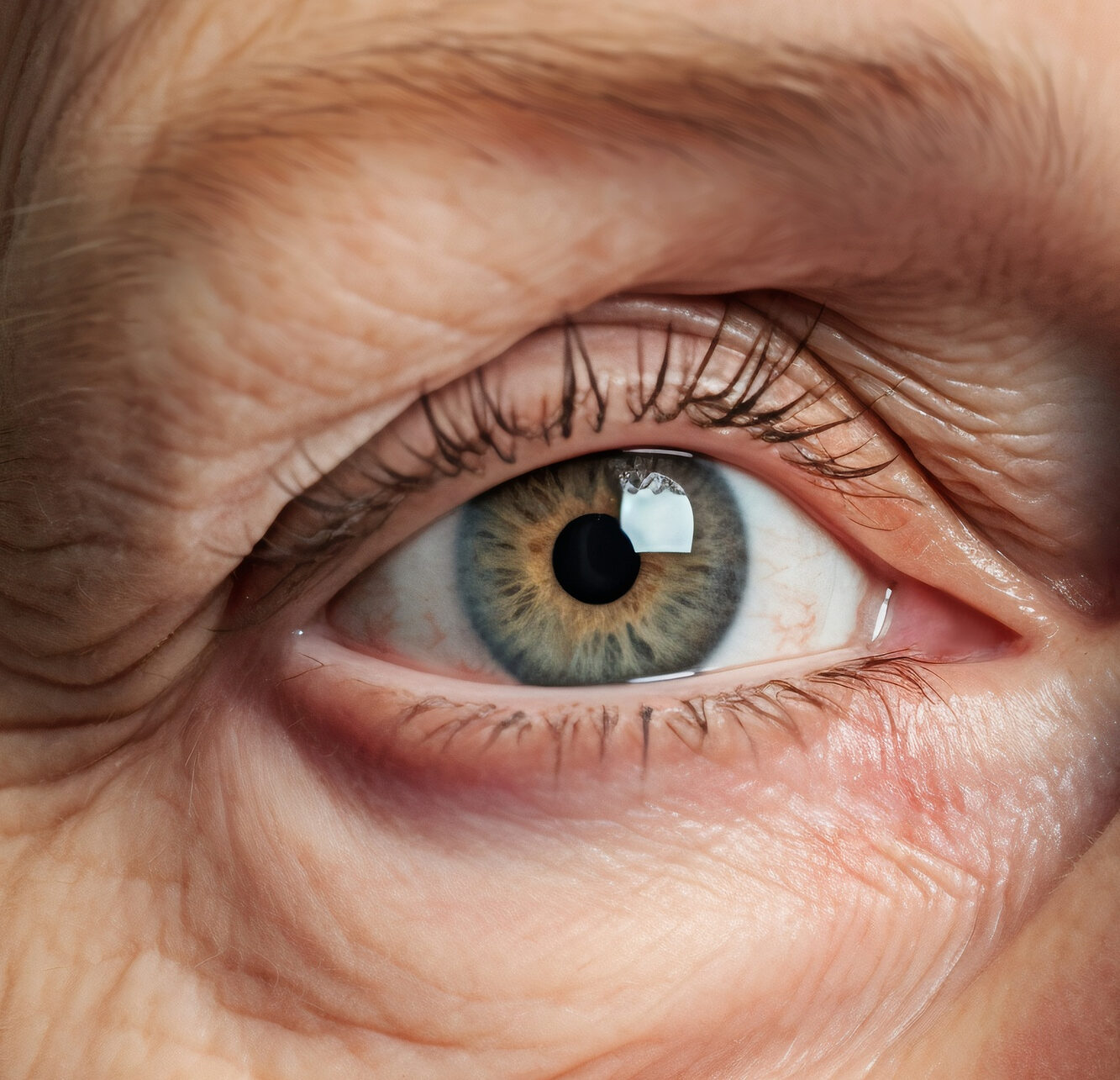
What is Eyelid Basal Cell Carcinoma?
Basal cell carcinoma (BCC) is a type of skin cancer. It is also known as a rodent ulcer and it is the most common type of skin and eyelid cancer.
BCCs most commonly occur when the cell DNA is damaged from exposure to ultraviolet (UV) radiation from the sun. It develops in the basal cells, which are in the outermost layer of the skin called the epidermis. The basal cells produce new skin cells as the old ones shed.
Elderly, fair-skinned adults who are naturally blond or red-haired with experienced sun damage and recurrent episodes of sunburn are more likely to develop Eyelid Basal Cell Carcinoma.
Exposure to ionising radiation and immune suppression due to disease or medicines can also increase cancer risk.
There are some rare inherited syndromes that predispose people to BCCs, such as basal cell naevus syndrome and xeroderma pigmentosum.

Is basal cell carcinoma on the eyelid serious?
Basal cell carcinomas (BCCs) account for most skin cancers around the eyes. While BCCs rarely spread to other parts of the body (metastases), they can be locally aggressive and invade neighbouring tissues.
What Types of Eyelid Basal Cell Carcinoma Are There?
BCC comes in various distinct clinical forms.
- Nodular BCC: The most common type on the eyelid that has a good prognosis if treated promptly.
- Infiltrative: it is the most aggressive one. It can be distinguished by thin cords of basaloid cells surrounded by a thick fibrotic stroma.
- Morphoeic: similar to Infiltrative BCCs, but they have smaller cell cords that are more angulated and extensively spread across the stroma.
- Mixed: Composed of nonaggressive and aggressive subtypes of BCCs.
BCCs can invade adjacent tissues and become ‘locally aggressive’. However, they do not spread to distant parts of the body.
What are the Causes of Eyelid Basal Cell Carcinoma?
There are risk factors that increase a person's chance of developing cancer but do not necessarily cause cancer directly. It is good to know if you have any risk factors, so that you may discuss them with your health provider and make better health choices.
- Fair Skin: when a person has less melanin, the skin's pigment, it provides less protection against UV radiation.
- Gender: the rates of skin cancer have increased in the recent years for men.
- Age: most basal cancers appear after the age of 50.
- Exposure to UV radiation: the sun produces two types of UVs: Ultraviolet A (UVA) & Ultraviolet B (UVB). UVB radiation produces sunburns and can be a cause of the development of cancer as it penetrates the skin more deeply.
- History of sunburn or fragile skin: having various episodes of sunburn or fragile skin from previous injuries or disease has a higher risk for eyelid cancer.
- Medical history: people with a weak immune system, taking certain medications, or having previous skin cancer can have a higher risk of developing eyelid cancer.
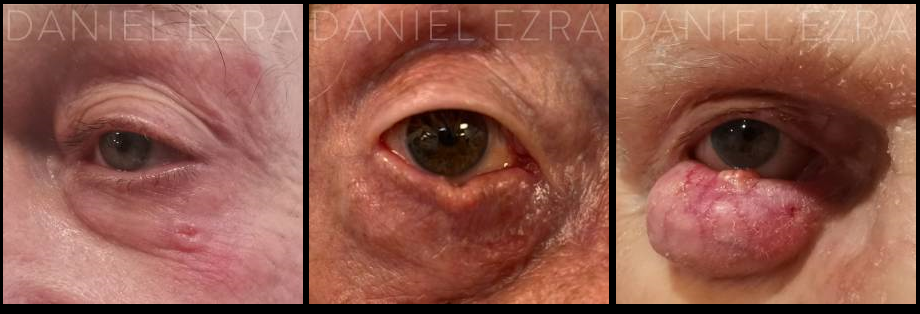
examples of Eyelid Basal Cell Carcinoma
Signs & Symptoms of Basal Cell Carcinoma?
Changes in your body may signal a problem that requires medical care.
BCCs usually present as a painless lump or spot on the eyelid which does not heal and gradually gets larger.
Other signs include:
- Loss of eyelashes where it grows
- Crusting or bleeding
- A notch in the eyelid margin
Tumour Diagnosis of Basal Cell Carcinoma/ When to see a doctor?
BCC is diagnosed when the doctor suspects that the lesion is a BCC by its appearance, and a biopsy (sample) is taken. The biopsy is sent to the laboratory for histological analysis, which can confirm whether it is a BCC, a different type of cancer or a benign lesion, such as a cyst.

TREATMENTS OPTIONS FOR EYELID BASAL CELL CARCINOMA
Most eyelid BCCs are treated with surgical excision.
Other forms of treatment, including cryotherapy, imiquimod cream, and radiotherapy, may be used to treat BCCs elsewhere in the body but are rarely used to treat BCCs on the eyelids unless unusual circumstances occur.
Several factors contribute to this, such as the risk of collateral eye damage and the advantage of having a histological examination of the specimen to confirm the diagnosis and ensure the margins are clear. If undergoing surgery, one can be more confident that the entire tumour has been removed.

Mohs Micrographic Surgery
The gold standard surgical technique for removing BCCs is Mohs micrographic surgery, described by Frederich Mohs. The tumour is removed and histologically analysed in this procedure by a Mohs dermatological specialist. They additionally examine the tumour's margins to ensure no tumour cells remain.
The eyelid reconstruction, which may be scheduled on the same day or a day or two later, is performed under local anaesthetic, either alone or with sedation, depending on the suspected size of the tumour and patient preference.
The Mohs surgeon will continue to remove tissue from the suspected region until s/he is confident there are no remaining tumour cells. The reconstruction is then performed by an oculoplastic surgeon (an eye surgeon specialising in the reconstruction of the eyelids and surrounding tissue).
Given the complex anatomy and functioning of the eyelid, an oculoplastic surgeon will use their skill and expertise to reconstruct the defect in the tissue, to make the eyelid as structurally and cosmetically normal as possible.
Excision with margins and immediate reconstruction
Some patients would prefer to have the tumour removed in one stage. Depending on the case, this option is reasonable, mainly if the tumour is a small, well-defined nodular BCC.
In this instance, the tumour is removed with a margin of healthy-looking tissue, typically 3mm. The reason for taking a margin of normal tissue is that tumours may extend a few millimetres beyond that microscopically. which is visible on the skin surface. The specimen is then sent to the laboratory, and the edges are examined to confirm that they are clear.
What are the advantages of Mohs for BCC
There is a reason for Mohs to be the most common micrographic surgery.
- Removes the cancer layer by layer
- Examines a much higher proportion of the specimen margin
- Lower rate of recurrence
- It minimises the amount of tissue removed, allowing a smaller wound


Before an Eyelid Basal Cell Carcinoma Treatment
How Can You Prevent Eyelid Basal Cell Carcinoma?
Once you have had one BCC, you have a 30-50% risk of developing another BCC within five years. Thus it is essential that you self-examine your skin regularly.
You can take further measures to avoid putting yourself at additional risk, including:
- Avoiding sun exposure, mainly when the sun is most intense (11 am to 3 pm)
- Regularly applying sunscreen containing both SPF and UVA protection
- Wearing UV protective sunglasses and a wide-brimmed hat
What Happens During an Eyelid Basal Cell Carcinoma Consultation?
How Should I Prepare for an Eyelid Basal Cell Carcinoma Treatment?
The Ezra Clinic - Reconstruction experts
The process of treating eyelid tumours is complex. We work closely with specialist Mohs dermatologists, who will remove the tumour whilst preserving the most tissue possible using a microscopic surgical technique.
The world-renowned surgeons at The Ezra Clinic specialise in eyelid reconstruction after removing the tumour.
These procedures are complex and will depend on the size and location of the tumour. We can offer a comprehensive set of treatments, and our extensive expertise in eyelid surgery means that we will focus not only on ensuring that the tissue is reconstructed with minimal impact on the eye and vision but also on ensuring the best possible aesthetic outcomes.
| Oculoplastic Surgeon | Plastic Surgeon | |
|---|---|---|
| Well trained in executing eyelid surgery | ✔ | ✔ |
| Trained to examine the eye | ✔ | X |
| Can examine the eye postoperatively to ensure that there are no eye related complications | ✔ | X |
| Can manage any eye related postoperative complications if they arise | ✔ | X |
Are there any risks associated with surgical treatment for Eyelid Basal Cell Carcinoma?
With any skin cancer removal, there is a very small risk that the tumour is not entirely removed or that it recurs. This risk is lowest with Mohs micrographic surgery but is also very low with surgical excision with margins.
Other risks of surgery to remove eyelid BCCs are the standard risks of any eyelid surgery. These risks are low but include visible scarring, bleeding, infection, and dry or watery eyes.
What are the complications/risks of Eyelid Basal Cell Carcinoma treatment/surgery?
With any skin cancer removal, there is a minimal risk that the tumour is not fully removed or recurs. This risk is lowest with Mohs micrographic surgery but low with surgical excision with margins.
Other risks of surgery to remove eyelid BCCs are the standard risks of any eyelid surgery. These risks are low but include visible scarring, bleeding, infection, and dry or watery eyes.
How much Does Treatment Cost?